Knee Pain Medicines and Tablets That Work: Types, Dosages, and More

Joint knee pain is one of the many diseases that afflict people in different parts of the globe. On the same note, a probable estimate forecasts one-quarter of the population of adults in the community saying they have ever had knee pain in their lifetime. Another source, namely the CDC, has also reported that a percentage of 10.4 of the entire U.S. adult population has osteoarthritis, which is the primary reason for knee pain. All these causes, for example, injuries, other forms of arthritis, and tendinitis affect the quality of life and, in most cases, result in a limited capacity to perform all activities.
Though most incidents of knee aches could be self-managed using rest, application of ice on the affected part, physiotherapy, and modifying one’s lifestyle, it is almost impossible in painful cases. A knee pain medicine may be useful in managing signs of the disorder and minimizing inflammation to allow the patient to return to his or her daily activities.
A person can take many knee pain medications, including in tablet form, topical form, or as an injection. Each may be more palatable or indicated for some genders, types, and causes of knee pain and can be delivered based on the patient’s health conditions, the severity of the pain, and their lifestyles. As regards the medicines that may be used to treat knee pain, their purpose, dosing, etc., the present guide will give further details so you can always act wisely and treat your knee pain effectively.
Understanding Knee Pain: Causes and Symptoms
Before diving into the medications, it’s essential to understand the common causes of knee pain and its symptoms:
- Osteoarthritis: Cartilage disease is a category of inflammatory diseases involving the bones and joints called osteoarthritis. During the condition, cartilage is broken due to inflammation, which opens the area for pain and stiffness.
- Rheumatoid Arthritis: A type of rheumatism that causes easy joint inflammation and causes pain, tightness, and swelling.
- Injuries: Acute or chronic knee pain will occur due to a ligament tear, a fracture or dislocation of any joint around the knee.
- Tendinitis: Day-to-day usage of the knee joint may lead to tendinitis, for instance, in athletes, in case the part becomes inflamed, leading to the voucher, which is known as pain.
Types of Knee Pain Medicine
With regard to the form and composition of such drugs, there are countless options for the treatment of knee pain that develops due to various causes and on various scales. To name a few, there are:
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
The first-line therapy, non pharmacological therapy of a patient suffering from knee pain, is NSAIDs because, in addition to being analgesia, they possess anti-inflammatory action. They work in the process of encouraging some chemicals in the human body by provoking Cyclooxygenase (COX), which causes tissue inflammation.
Common NSAIDs for Knee Pain:
a) Ibuprofen (Advil, Motrin): Present in oral liquid medications and in tablet and capsule forms to be purchased over the counter or by prescription.
b) Aleve, Naprosyn Other nonprescription medications in the same group as Advil and which circulate for longer in the bloodstream include Naproxen.
c) Diclofenac (Voltaren): Available as a tablet and gel and preferred for topical uses and pain relief with less effect on the whole body and side effects.
Dosage and Usage:
a) For Ibuprofen: This can be given in 200-400 mg every 4-6 h, in regard to the severity of the patient's pain and should not be administered with a maximum daily dose of 3200 mg.
b) For Naproxen: The conventional dose of enalapril is 220mg; this has to be taken three to four times a day depending on the degree of severity, and it should probably take a maximum of 660mg per day.
c) For Diclofenac (topical gel): One has to uniquely apply between 2 and 4 grams and massage gently the aching knee thrice or four times daily.
Side Effects:
Long-term side effects of NSAIDs include stomach discomfort or upset, ulcers, and kidney issues. In other words, the least amount that can be effective is the most desired for the shortest possible duration is the best.
2. Acetaminophen (Paracetamol)
Paracetamol is an analgesic without an Anti-inflammatory property; its sole property is to relieve pain. It is used in those patients who are contraindicated to NSAIDs because of gastrointestinal or renal complaints.
Common Brands: Tylenol, Panadol
Dosage and Usage:
It should be taken in 500–1000 mg every 4–6 hours when necessary unless 400 mg is taken per day.
Side Effects:
It is generally regarded as safe and well, and that penetrates the liver barrier well; however, it is toxic to the liver if administered in large dosages. Since this medicine has a hepatotoxic effect, alcohol is discouraged while taking this medicine.
3. Corticosteroids
However, there are other powerful anti-inflammatories, such as corticosteroids, which doctors mainly prescribe when the knee pain is severe and caused mostly by arthritis. Sometimes, oral steroids or systemic or intra-articular steroids may be administered.
Common Corticosteroids for Knee Pain:
a) Prednisone: A prescription oral medicine for the treatment of serious inflammation.
b) Methylprednisolone (Depo-Medrol, Medrol): This can be prepared as an oral solution or in a form to be administered for intro-arthrocentesis or in the form of an injection for the knee joint.
Dosage and Usage:
a) Oral Prednisone: Normally, its range is 5-60mg a day, but it will depend on the efficacy and tolerance of the patient.
b) Injectable Methylprednisolone: Usually 20-80 mg, intra-articular injection under contraindication of using it more than once in 3–6 months as due to this, the cartilage level may get depleted.
Side Effects:
Among the side effects of corticosteroids that are considered to be long-term effects are heartburn, increase in weight and blood pressure, osteoporosis and damage to the joints. In turn, simple sequencing mandates the optimization of injection depending on the occurrence of joint complications.
4. Disease-modifying anti-rheumatic Drugs (DMARDs)
DMARDs are drugs that are most likely medicines that have been used to treat autoimmune diseases such as rheumatoid arthritis. This family of medicines prevents the immune system from responding again to the joints, physiologically escalating knee pain and inflammation.
Common DMARDs:
a) Methotrexate: Of all the treatment possibilities, it is one of the most popular for rheumatoid arthritis.
b) Hydroxychloroquine (Plaquenil): Often advised to be used for minor cases or together with other therapies.
Dosage and Usage:
a) Methotrexate: It is prescribed in weekend doses starting from 7,5 to 25 Mg depending on the reaction of the patient.
b) Hydroxychloroquine is used as an extra 200-400 mg a day.
Side Effects:
Some of the SSCs which may present complications include hepatotoxicity, gastrointestinal intolerance, and immunosuppression. Since the drug will operationalise in the blood, constant blood tests are necessary in monitoring this medicine.
5. Opioids
Opioids are analgesic solid pain medicines and are prescribed strictly for severe knee pain when the other drugs have not worked. They act by acting on opioid receptor sites in the brain and, therefore, are associated with a decrease in the feeling of pain.
Common Opioids for Knee Pain:
a) Tramadol: A weaker opioid analgesic that can be regularly used for middle-level knee pain.
b) Oxycodone and Morphine: New generations of strong opioids for administration for pain that cannot be controlled adequately otherwise.
Dosage and Usage:
a) Tramadol: D: 50–100 mg every 4–6 hours ‘as needed’; maximum daily dose: 400 mg.
b) Oxycodone: In patients with moderate to severe pain, 5–10 mg every 4–6 hours as required, given the nature of pain.
Side Effects:
Opioids pose risks similar to the dec…the side effects include drowsiness, constipation, nausea, and addiction if the drug is used for a long time. They should only be taken under medical supervision since they pose significant patient threats.
Knee pain drugs also vary in form and strength, as drugs work based on the etiology as well as the severity of the disease. The drug called mild will be an analgesic, while the strong one will be an anti-inflammatory one. The following table summarizes the most common drugs for knee pain, dosages, and side effects:
|
Type of Medicine |
Common Medications |
Dosage & Usage |
Side Effects |
|
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) |
Ibuprofen (Advil, Motrin), Naproxen (Aleve, Naprosyn), Diclofenac (Voltaren) |
- Ibuprofen: 200–400 mg every 4–6 hours, max 3200 mg/day - Naproxen: 220 mg every 8–12 hours, max 660 mg/day - Diclofenac (Topical Gel): Apply 2–4 grams 4x/day |
Stomach upset, ulcers, kidney issues (long-term use). |
|
2. Acetaminophen (Paracetamol) |
Tylenol, Panadol |
500–1000 mg every 4–6 hours as needed, max 4000 mg/day |
Liver toxicity at high doses, especially with alcohol use. |
|
3. Corticosteroids |
Prednisone, Methylprednisolone (Depo-Medrol, Medrol) |
- Prednisone: 5-60 mg/day - Methylprednisolone: 20-80 mg injected into the knee once every 3–6 months |
Weight gain, high blood pressure, osteoporosis, joint damage (if overused). |
|
4. Disease-modifying anti-rheumatic Drugs (DMARDs) |
Methotrexate, Hydroxychloroquine (Plaquenil) |
- Methotrexate: 7.5-25 mg weekly - Hydroxychloroquine: 200-400 mg daily |
Liver toxicity, gastrointestinal issues, immune suppression. |
|
5. Opioids |
Tramadol, Oxycodone, Morphine |
- Tramadol: 50-100 mg every 4-6 hours, max 400 mg/day - Oxycodone: 5-10 mg every 4-6 hours |
Drowsiness, constipation, nausea, dependency (long-term use). |
Topical Solutions for Knee Pain
It can be applied to the affected knee to limit side effects typically associated with systemic intake. Heretofore, these drugs were administered to patients whose pain was not severe and/ or who were concurrently taking other oral analgesics.
1. Topical NSAIDs
Dynamic fixings in "counterirritant" creams incorporate methyl salicylate, which can make the sensation of burning or cooling draw consideration absent from the torment.
- Application: Apply a thin gel layer to the affected knee as much as four times daily. Follow the label's dosage instructions.
2. Capsaicin Cream
Capsaicin cream comes from chillies; it draws out P, which is a pain-transmitting chemical in the body.
- Application: Use topically to the knee joint; use 3–4 times a day; it may take several days for pain relief to be noticeable.
- Side Effects: Capsaicin cream can cause burning initially, after which an application should be washed off hands carefully to avoid your eyes or mucous membranes.
3. Lidocaine Patches or Creams
It is a local anesthetic capable of temporarily numbing the region to which it is administered in order to dull the pain signals so that they are not allowed to reach the brain, thus making it efficient in eradicating acute pain and even beneficial to patients who suffer from chronic knee osteoarthritis.
- Application: Apply a lidocaine patch or cream to the painful area for 12 hours once a day. Patches may be cut to fit over the knee joint area.
- Side Effects: This medication can cause skin irritation or a slight burning sensation. Avoid using it on broken or irritated skin.
4. Methyl Salicylate Creams (Counterirritants)
Dynamic fixings in "counterirritant" creams incorporate methyl salicylate, which can make the sensation of burning or cooling draw consideration absent from the torment. Brands with this ingredient include Bengay and Icy Hot, whose use typically describes relief from joint pain.
- Application: Apply small amounts of cream to the knee area 3-4 daily after a gentle massage. Do not apply the area with heat wraps, or someone else may burn.
- Side Effects: Irritation or redness of the skin can occur, especially if used with another source of heat. Handwashing after application is to be done.
5. Menthol-Based Gels
Yet another cooling agent is menthol, which is derived from mint and provides a cooling sensation. Thus, knee pain may be relieved through the stimulation of receptors in the skin from menthol. It usually comes with other components like camphor in the products bearing Bio-freeze.
- Application: Apply a lean layer of menthol gel around the knee 3–4 times a day. The impact endures for some hours and is for short-term alleviation.
- Side Effects: There may be a slight bothering on the skin, particularly to delicate parts. Dodge touching the eyes or any broken skin.
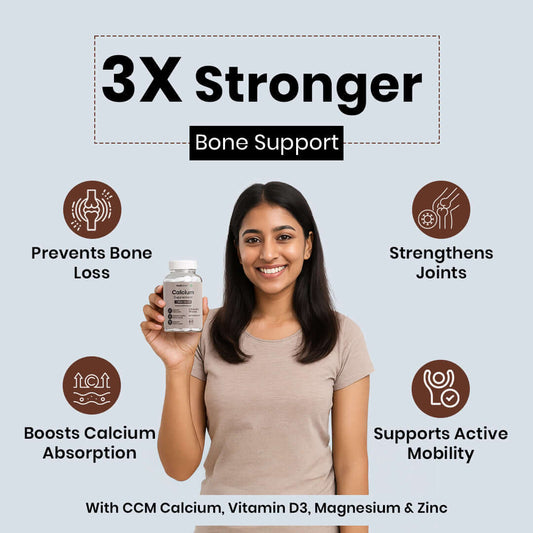
Supplements for Knee Pain
A few supplements are advantageous to people suffering from knee torment, particularly in case the cause of the issue is osteoarthritis. They don't serve to diminish the degree of torment expediently but can help in solid joints over time.
1. Glucosamine and Chondroitin
Glucosamine and chondroitin help stop joint cartilage from breaking down, which can help slow down osteoarthritis.
- Dosage: Generally, 1500 mg of glucosamine and 1200 mg of chondroitin are needed daily.
2. Omega-3 Fatty Acids
Curcumin found in turmeric has properties that reduce inflammation and might lower knee pain.
- Dosage: It is usually recommended to take 500 to 1000 mg of curcumin extract each day, with black pepper added to improve absorption.
3. Turmeric and Curcumin
Curcumin, the active compound in turmeric, has been studied for its anti-inflammatory effects and could help reduce knee pain.
- Dosage: Take 500 to 1000 mg of curcumin extract daily, with black pepper added to increase absorption.
4. Methylsulfonylmethane (MSM)
MSM is a sulfur-based compound that may help lower pain, especially in osteoarthritis patients. It can reduce swelling and improve joint flexibility.
- Dosage: 1000 to 3000 mg daily, usually taken in two or three doses.
5. Boswellia Serrata, or Indian Frankincense
Boswell is a plant supplement known for its strong anti-inflammatory effects. It may be an easy and effective option for reducing pain and swelling in arthritis cases. It functions by blocking the creation of leukotrienes, which are believed to trigger inflammation.
- Dosage: It is recommended to take this supplement 1-3 times daily, with a total amount of 100-200 mg of Boswell extract that is standardized to 60% Boswell acids.
A couple of supplements have been added to support joint health and alleviate knee aches, especially during osteoarthritis. These supplements do not cure the problem, but they conclude with a more extended functional or low-inflammation phase for the joint capsule.
|
Supplement |
Benefit |
Dosage |
|
Glucosamine and Chondroitin |
It may moderate the movement of osteoarthritis and ensure joint cartilage. |
1200 mg of chondroitin and 1500 mg of glucosamine per day. |
|
Omega-3 Fatty Acids |
bring down irritation and advance the common well-being of the knee joint.
|
1000 mg of omega-3 greasy acids or angle oil each day. |
|
Turmeric and Curcumin |
The solid anti-inflammatory properties of curcumin may help reduce knee torment. |
500–1000 mg of black pepper and curcumin extract per day. |
|
Methylsulfonylmethane (MSM) |
Lessens pain and inflammation and may increase osteoarthritis joint suppleness. |
1000–3000 mg daily, split into two or three doses. |
|
Boswellia Serrata |
It is well-known for lowering pain and swelling because of its anti-inflammatory qualities. |
One to three times a day, 100–200 mg standardized to 60% boswellic acids. |
Injectable Treatments for Knee Pain
Injectable treatment can be resorted to if the topical and oral treatments cannot help alleviate the situation. A healthcare provider administers these treatments
1. Corticosteroid Injections
This medicine actuates such a solid anti-inflammatory reaction on the knee joint that the torment, swelling, and redness all scatter. In a few occurrences, there's the help of torment, which dies down within days. Corticosteroid infusions are regularly endorsed for the essential reason of anti-inflammatory in a number of infections influencing the joints, including rheumatoid joint pain and osteoarthritis. All things considered, rehashed infusions are too likely to bring almost a number of destructive impacts, counting slow debilitating or harm to the cartilage.
2. Hyaluronic Acid Injections
Hyaluronic corrosive infusion imitates liquid alter within the knee joint. The liquid of the knee joint is misplaced with maturing or illnesses like osteoarthritis. This diminishes contact between bone and bone, soothing the related torment and distress, and increases joint mobility. In order to preserve the joint's long-term wellbeing and usefulness, hyaluronic corrosion will continuously advance nearby synovial liquid generation.
- Dosage and Usage: Typically administered once weekly for 3–5 weeks. Results may last several months.
3. Platelet-Rich Plasma (PRP) Therapy
The concept behind PRP treatment is basic:
it consists of drawing profoundly concentrated platelets from the patient's blood, which would contain development variables advancing the repair of harmed tissues within the knee. Treatment for harmed cartilage, tendinitis, and tendons progress joint work, mends harmed tissue and diminishes irritation. The lion's share of the patients feel that a few infusions of PRP have caused them to be pain-free and made strides in portability.
- Dosage and Administration: Usually, one to three injections are required to be given intermittently over a couple of weeks.
4. Prolotherapy (Proliferation Therapy)
Prolotherapy may be a portion of regenerative pharmaceuticals. It infuses an arrangement or, more frequently, dextrose into the knee joint or the connective tissues and tendons that shape the knee joint. Additionally, it can cause the cells to move in reverse and incite the body's common self-repairing instrument. People who confront issues of long-standing precariousness within the knee incredibly advantage from prolotherapy since it is one treatment that will decrease torment coming about from wounds and conjointly revitalize the tendons and ligaments.
- Dosage and Usage: Generally, the treatment is carried out through a number of injections, between three and six at a week's interval, depending on the intensity of the patient’s condition.
5. Stem Cell Injections
One such new treatment age is the form of stem cell therapy, where cells can be injected into the knee joint, further enhancing the repairing and rejuvenating processes for any damaged cartilage, tissues, and healing procedure. Cells can be drawn from the patient's body, such as bone marrow, adipose, or donated umbilical cord tissue. These are particularly useful in cases of knee osteoarthritis as well as any conditions where injury to the cartilage results in damage or degeneration of a joint for which other interventions may not work.
- Dosage and Usage: Typically, stem cell injections require one or two sessions, with the possibility of follow-up injections depending on the severity of the knee condition.
Dosage and Safety Tips for Knee Pain Medicines
- Consult with a Healthcare Provider: It is always advisable for anyone with a chronic disease to seek advice from a doctor on what kind of drug to take.
- Follow Dosage Guidelines: It is also important not to take more of knee pain medicine as it triggers specific side effects.
- Monitor for Side Effects: Be aware of side effects. Report any symptoms or illness you have never felt to the doctor.
- Consider Non-Medication Therapies: Patients were also saying that this pain can be relieved without medication through physical therapy, exercise, or by simply implementing lifestyle changes instead of prescriptions.
Conclusion
Given the many analgesics available for knee pain, the right treatment would still be withheld depending on what is causing the pain, its severity and duration, and the existing medical condition. It is always possible to manage and prevent knee pain by using different types of NSAIDs, acetaminophen, corticosteroids, and opioids; in cases of inflammation or autoimmune diseases, DMARDs and injectables are used. Other nutrients such as glucosamine and chondroitin also aid in joint health in the long run, and if they are positive, turmeric can also be an option.
However, all these medicines require strict medication by a doctor and proper dosages and precautions to avoid side effects.
References
1. American College of Rheumatology. (2020). Osteoarthritis Treatment: Nonsteroidal Anti-Inflammatory Drugs (NSAIDs). Retrieved from https://www.rheumatology.org
2. Mayo Clinic. (2023). Acetaminophen (Tylenol). Retrieved from https://www.mayoclinic.org
3. National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). (2022). Corticosteroid Injections for Knee Pain. Retrieved from https://www.niams.nih.gov
4. National Rheumatoid Arthritis Society. (2021). Disease-Modifying Anti-Rheumatic Drugs (DMARDs). Retrieved from https://www.nras.org.uk
5. U.S. National Library of Medicine. (2021). Opioids for Pain Relief: Risks and Side Effects. Retrieved from https://medlineplus.gov
6. Cleveland Clinic. (2023). Hyaluronic Acid Injections for Knee Osteoarthritis. Retrieved from https://my.clevelandclinic.org
7. Arthritis Foundation. (2023). Understanding Glucosamine and Chondroitin for Osteoarthritis. Retrieved from https://www.arthritis.org
8. Healthline. (2021). Omega-3 Fatty Acids for Joint Health. Retrieved from https://www.healthline.comNo comments





















0 comments