The Pancreas–Diabetes Connection: How This Tiny Organ Controls Your Blood Sugar
When we consider organs which sustain us, our heart and lungs tend to hog all the limelight. However, there's a small, soft organ working silently in the background to make you healthy: the pancreas.
It might be small when weighed next to the heart or liver, but it has a giant function in one of your body's most crucial tasks — regulating your blood sugar level.
Blood glucose control isn't merely a matter of not eating sweets or forgoing dessert. It's the way your body processes food for energy, stores that energy, and has it available when you need it. It's all connected to your pancreas's function to make and control insulin. And if the pancreas isn't working efficiently, diabetes can occur.
Here, in this article, we'll deconstruct how the pancreas function works, its relationship to diabetes causes, the meaning of insulin resistance, how pancreatic health affects your entire body, and what you can do — including supplements — to help it.
Understanding the Pancreas Function
The pancreas is a deep abdominal gland, sitting between your stomach and spine. Although it is small, it performs two very important functions:
- Digestive function – secreting enzymes to break down protein, fat, and carbohydrates.
- Endocrine function – secreting hormones into your blood, the most well-known being insulin and glucagon.
Located within the pancreas are groups of cells named islets of Langerhans. Within the islets, beta cells are tasked with the special responsibility of making insulin. This hormone instructs your cells to take in glucose from your blood and utilize it for energy. Without insulin, glucose cannot enter your cells, leaving excess sugar in your blood.
Imagine your pancreas as your body's blood sugar "thermostat." A thermostat regulates the perfect room temperature, and your pancreas regulates proper blood glucose levels.
Pancreas and Diabetes Link
The relationship between the pancreas and diabetes is simple but serious:
When your pancreas is unable to make sufficient insulin, or
When your body is resistant to insulin, your blood sugar levels increase, resulting in type 2 diabetes or even type 1 diabetes in some circumstances.
If your pancreas health worsens — for example, through inflammation, infection, autoimmune attack, or damage from lifestyle choices — your beta cells can become weak or even die. Consequently, blood sugar levels remain high for extended periods, leading to damage of nerves, blood vessels, and organs.
Early signs of blood sugar difficulties associated with the pancreas are:

- Increased thirst
- Frequent urination
- Fatigue
- Slow healing of wounds
- Unusual weight changes
Dismissing these warning signs can result in more serious complications.
Insulin Production and Blood Sugar Regulation
Your pancreas is the sole organ responsible for making insulin, so it is indispensable when it comes to controlling blood sugar levels.
Here's how it works:
- You consume a meal – Your food is digested into glucose (sugar).
- Blood sugar increases – Your pancreas detects this fluctuation.
- Release of insulin – Beta cells release insulin into your blood.
- Glucose uptake – Insulin behaves like a key, opening your cells so glucose can gain entry and be used for glucose metabolism (energy production).
- Blood sugar levels stabilize – When they return to normal, insulin release slows.
When this process goes well, you are full of energy and stable. Yet if the production of insulin ceases or your body no longer responds to insulin, glucose remains in your bloodstream — resulting in hyperglycemia (high blood sugar).
Insulin Resistance and Diabetes Causes
Insulin resistance happens when your cells stop responding to insulin’s “open up” signal. Imagine knocking on a door repeatedly, but no one lets you in — that’s what happens to glucose during insulin resistance.
Main diabetes causes linked to pancreas function include:
- Poor diet – High in sugar, refined carbs, and unhealthy fats.
- Lack of physical activity – Reduces your body’s ability to use glucose effectively.
- Chronic stress – Stress hormones can interfere with insulin function.
- Obesity – Excess fat, especially around the abdomen, worsens insulin resistance.
-
Genetics – Family history can predispose you to pancreatic and blood sugar issues.
If not addressed, insulin resistance can silently progress to type 2 diabetes, putting you at risk for heart disease, kidney problems, and nerve damage.
Pancreatic Disorders and Their Impact
When pancreatic health is compromised, blood sugar regulation suffers. Some common pancreatic disorders include:
- Pancreatitis – Inflammation that can damage insulin-producing cells.
- Pancreatic cancer – Sometimes disrupts hormone production.
- Cystic fibrosis – Thick mucus blocks pancreatic enzyme flow.
These conditions directly affect insulin production and glucose metabolism. Even mild, chronic inflammation can reduce your pancreas’s efficiency, leading to persistent high blood glucose levels.
Pancreatic Hormones Beyond Insulin
While insulin gets the spotlight, your pancreas also produces glucagon — insulin’s opposite. When your blood sugar drops too low, glucagon signals your liver to release stored glucose back into the blood.
Other hormones, like somatostatin and pancreatic polypeptide, help fine-tune digestion and hormone balance, showing that your pancreas does more than just manage sugar.
Diabetes Prevention Through Pancreatic Health
You can protect your pancreas and lower your risk of type 2 diabetes by focusing on:
Diet tips:
- Eat high-fiber foods like whole grains, fruits, and vegetables.
- Limit processed sugar and refined carbs.
- Include lean proteins and healthy fats.
Exercise:
- Engage in at least 30 minutes a day of moderate exercise to improve glucose metabolism.
- Strength training improves insulin sensitivity.
Regular checks:
- Check fasting blood sugar annually.
- And if you have a family history of diabetes, test more often.
Best Supplements to Control Blood Sugar and Support Pancreatic Health
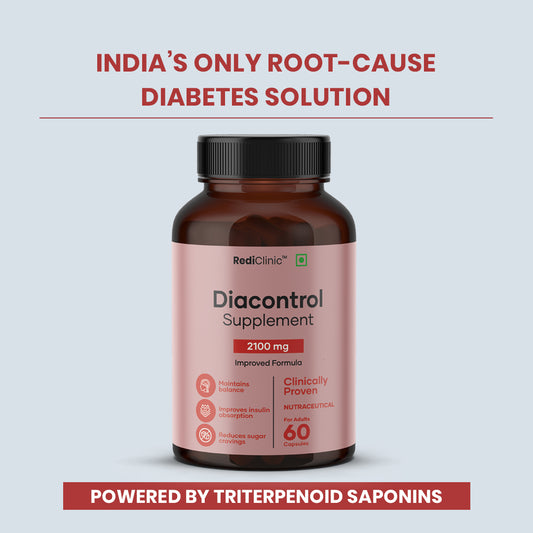
Where diet and lifestyle are the cornerstone, there are some supplements that can offer additional support for blood sugar and pancreatic function. Some of the best-researched alternatives follow — a consideration of RediClinic DiaControl, an herbal specialty blend among them:
- Chromium – Enhances insulin action and improves glucose metabolism, helping cells absorb sugar more efficiently.
- Magnesium – Low magnesium levels are linked to insulin resistance. Supplementing may improve insulin sensitivity and overall metabolic function.
- Alpha-lipoic acid (ALA) – A powerful antioxidant that can protect beta cells from damage and enhance insulin sensitivity.
- Cinnamon extract – Contains compounds that may lower fasting blood glucose levels and improve carbohydrate metabolism.
-
Gymnema sylvestre – Nicknamed the “sugar destroyer,” it supports pancreatic health, curbs sugar cravings, and can assist in reducing glucose absorption in the intestines.
RediClinic DiaControl – Natural herbal supplement designed to help maintain blood glucose levels under control and support the natural function of the pancreas.

Click Here To Buy From Our Official Website
Key Ingredients & Actions:
The below are the few ingredients to control blood sugar levels and how rediclinic diacontrol supplement works for pancreas to release insulin to reduce diabetes in body:
- Gymnema sylvestre – Aids in inhibiting sugar absorption and enhancing insulin action.
- Cinnamomum camphora (Cinnamon) – Increases insulin sensitivity and regulates blood sugar metabolism.
- Momordica charantia (Bitter Melon) – A natural metabolism assistant for sugar.
- Pterocarpus marsupium (Vijaysar) – Famous to make the pancreas regenerate.
- Berberis aristata – Normalizes glucose metabolism and gut health.
How It Works: DiaControl works on three levels — improving insulin sensitivity, supporting beta cell health, and balancing post-meal sugar spikes.
Why It Stands Out: Its multi-ingredient approach combines time-tested Ayurvedic herbs with modern formulation standards, making it suitable for long-term use as part of a healthy lifestyle.
Important: Always consult your healthcare provider before starting any supplement, especially if you are on diabetes medication, to avoid potential interactions or low blood sugar episodes.
Frequently Asked Questions (FAQs)
1. Is diabetes reversible through pancreatic health improvement?
In the initial phase of type 2 diabetes, enhancing diet, exercise, and insulin resistance reduction can greatly enhance blood sugar control. Complete reversal, however, is determined by one's health conditions.
2. What is the ideal diet to regulate blood glucose?
An appropriate diet consisting of low-glycemic index foods, vegetables in abundance, whole grains, lean protein, and healthy fat serves best.
3. How do I know if I have insulin resistance?
Normal signs are belly fat, having to eat all the time, tiredness, and darkening of the skin around your neck or underarm area. Blood tests will verify it.
4. Which foods hurt the pancreas?
Extremely processed food, soda, too much alcohol, and fried foods can cause harm to the pancreas.
5. Are supplements okay to take long-term?
When used at recommended dosages and with medical supervision, most supplements are safe. Natural is not always risk-free.
Conclusion
Your pancreas may be small, but it has an enormous impact on your health. By understanding how it works, recognizing the signs of trouble, and making conscious choices in diet, exercise, and supplementation, you can protect your pancreatic health, maintain balanced blood glucose levels, and reduce your risk of type 2 diabetes.
Take care of this tiny organ, and it will take care of you for years to come.
No comments



















0 comments